
This AOP is licensed under the BY-SA license. This license allows reusers to distribute, remix, adapt, and build upon the material in any medium or format, so long as attribution is given to the creator. The license allows for commercial use. If you remix, adapt, or build upon the material, you must license the modified material under identical terms.
AOP: 468
Title
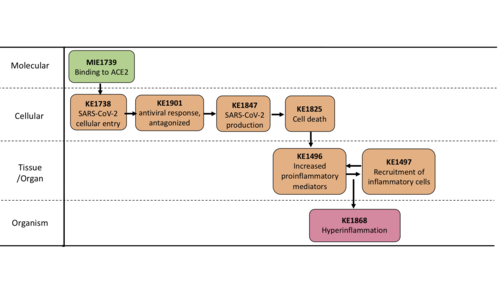
Binding of SARS-CoV-2 to ACE2 leads to hyperinflammation (via cell death)
Short name
Graphical Representation
Point of Contact
Contributors
- Laure-Alix Clerbaux
- Penny Nymark
- Sabina Halappanavar
- Sally Mayasich
Coaches
OECD Information Table
| OECD Project # | OECD Status | Reviewer's Reports | Journal-format Article | OECD iLibrary Published Version |
|---|---|---|---|---|
This AOP was last modified on April 29, 2023 16:03
Revision dates for related pages
| Page | Revision Date/Time |
|---|---|
| Binding to ACE2 | October 21, 2024 02:25 |
| SARS-CoV-2 cell entry | April 04, 2023 07:39 |
| Interferon-I antiviral response, antagonized by SARS-CoV-2 | December 15, 2023 14:27 |
| Increased SARS-CoV-2 production | June 14, 2022 08:49 |
| Increase, Cell death | November 27, 2024 11:26 |
| Increased, secretion of proinflammatory mediators | May 17, 2023 15:18 |
| Increased, recruitment of inflammatory cells | May 12, 2023 17:03 |
| Hyperinflammation | December 29, 2021 02:29 |
| Binding to ACE2 leads to SARS-CoV-2 cell entry | October 21, 2024 02:55 |
| Recruitment of inflammatory cells leads to Increased proinflammatory mediators | September 01, 2022 03:51 |
| SARS-CoV-2 cell entry leads to IFN-I response, antagonized | December 12, 2023 15:15 |
| IFN-I response, antagonized leads to SARS-CoV-2 production | December 14, 2023 15:23 |
| SARS-CoV-2 production leads to Increase, Cell death | October 19, 2021 13:39 |
| Increase, Cell death leads to Increased proinflammatory mediators | September 01, 2022 03:49 |
| Increased proinflammatory mediators leads to Recruitment of inflammatory cells | May 18, 2023 12:46 |
| Recruitment of inflammatory cells leads to Hyperinflammation | February 08, 2023 09:25 |
Abstract
In lungs, SARS-CoV-2 Spike (S) proteins bind to the Angiotensin 2 Converting Enzyme (ACE-2) receptor (KE1739, Binding to ACE2), expressed at high levels on airway epithelial cells, alveolar epithelial cells, vascular endothelial cells and macrophages. Upon binding, the S protein subunits undergo sequential cleavage mediated by proteases and conformational changes that results in virus and host cell membrane fusion and viral entry into the cells (KE1738, SARS-CoV-2 cellular entry). Following cellular entry, the SARS-CoV-2 virus has evolved a repertoire of proteins that block the interferon cascade so the host antiviral proteins are not expressed, and the virus is free to replicate. If the type I interferon antiviral response is antagonized (KE1901, Interferon-I antiviral response antagonized by SARS-CoV-2), the viral RNA can be translated, replicated, transcribed and the genomic RNA packaged before the new SARS-CoV-2 virions are assembled (KE1847, SARS-CoV-2 production). SARS-COV-2 is a cytopathic virus and causes massive cell death in lungs (KE1825, Increased cell death). Cell death triggers immune response. Activated local innate immune response includes secretion of soluble factors such as cytokines (IL-6, TNF), chemokines (CXCL8), growth factors, hormones and several types of metabolites (KE1496, Increased secretion of pro-inflammatory mediators). This KE is the most common/central node common of the network. The soluble factors recruit immune cells including macrophages, monocytes and lymphocytes to the sites of infection (KE1497, Recruitment of immune cells), which further amplify secretion of cytokines and chemokines, creating a pro-inflammatory environment. Prolonged and self-perpetuating inflammatory response referred to as hyperinflammation (KE1866, Hyperinflammation) exhibiting notably excessive serum levels of pro-inflammatory mediator C-reactive protein (CRP). A vicious cycle of hyperinflammatory response initiated by SARS-CoV-2 leads to tissue injury, pulmonary dysfunction and organ failure.
AOP Development Strategy
Context
This AOP is developed within the CIAO project, "Modelling the Pathogenesis of COVID-19 Using the Adverse Outcome Pathway (AOP)". The overall goal is to organize and understand the vast amount of data that is constantly evolving as a result of the COVID-19 pandemic. This AOP-aligned systematic organisation of the knowledge allows to identify uncertainties and knowledge gaps. Many AOPs were developed in the CIAO project, each AOP focusing on a specific element of the SARS-COV-2 virus responses in humans.
This AOP focuses on the acute respiratory distress associated mortality following viral infection of pulmonary cells by SARS-CoV-2 leading to cell death and excessive inflammatory repsonse.
Strategy
Summary of the AOP
Events:
Molecular Initiating Events (MIE)
Key Events (KE)
Adverse Outcomes (AO)
| Type | Event ID | Title | Short name |
|---|
| MIE | 1739 | Binding to ACE2 | Binding to ACE2 |
| KE | 1738 | SARS-CoV-2 cell entry | SARS-CoV-2 cell entry |
| KE | 1901 | Interferon-I antiviral response, antagonized by SARS-CoV-2 | IFN-I response, antagonized |
| KE | 1847 | Increased SARS-CoV-2 production | SARS-CoV-2 production |
| KE | 1825 | Increase, Cell death | Increase, Cell death |
| KE | 1496 | Increased, secretion of proinflammatory mediators | Increased proinflammatory mediators |
| KE | 1497 | Increased, recruitment of inflammatory cells | Recruitment of inflammatory cells |
| AO | 1868 | Hyperinflammation | Hyperinflammation |
Relationships Between Two Key Events (Including MIEs and AOs)
| Title | Adjacency | Evidence | Quantitative Understanding |
|---|
| Binding to ACE2 leads to SARS-CoV-2 cell entry | adjacent | High | High |
| SARS-CoV-2 cell entry leads to IFN-I response, antagonized | adjacent | High | Moderate |
| IFN-I response, antagonized leads to SARS-CoV-2 production | adjacent | High | Moderate |
| SARS-CoV-2 production leads to Increase, Cell death | adjacent | High | Moderate |
| Increase, Cell death leads to Increased proinflammatory mediators | adjacent | ||
| Increased proinflammatory mediators leads to Recruitment of inflammatory cells | adjacent | High | High |
| Recruitment of inflammatory cells leads to Hyperinflammation | adjacent |
Network View
Prototypical Stressors
Life Stage Applicability
Taxonomic Applicability
Sex Applicability
Overall Assessment of the AOP
Domain of Applicability
Essentiality of the Key Events
Evidence Assessment
Known Modulating Factors
| Modulating Factor (MF) | Influence or Outcome | KER(s) involved |
|---|---|---|
| Sex |
Higher risk for severe AO for males |
2056, 1703, 2354 |
| Age |
risk for more severe AO increases with age |
2056, 1703, 2354 |
| Obesity | risk for more severe AO increases linearly with BMI increase, already starting at BMI >23 kg/m2 | 2056, 1703, 2354 |
| Vit D deficiency | Low vitamin D status prior to infection increases risk of higher AO severity | 2056 , 1703, 2354 |
| Chemicals (PFAS, PFOS, PFOA, PFNA, PFHxS, and GenX) | chemical exposure correlates with higher risk for AO severity | 2056, 1703, 2354 |